Special Populations Require Special Planning
Pandemics, Biological and Chemical Incidents
All healthcare facilities must have a state-reviewed Emergency Preparedness Plan (EPP) that explains how to shelter in place and protect patients/residents during crises. How familiar are you with yours? How well did it work during the recent Covid-19 Pandemic? Judging from mortality rates, it could have worked better in NY, NJ and CA. A pandemic can easily be a multi-year event. Moreover, pandemics don't disappear if countries keep financing "gain of function" research to weaponize viral pathogens like Covid-19. While hospitals can't stop that, they can be better prepared to deal with the created pandemic crises, avoiding preventable deaths, staff absenteeism, school disruptions, job losses, and global economic downturns.
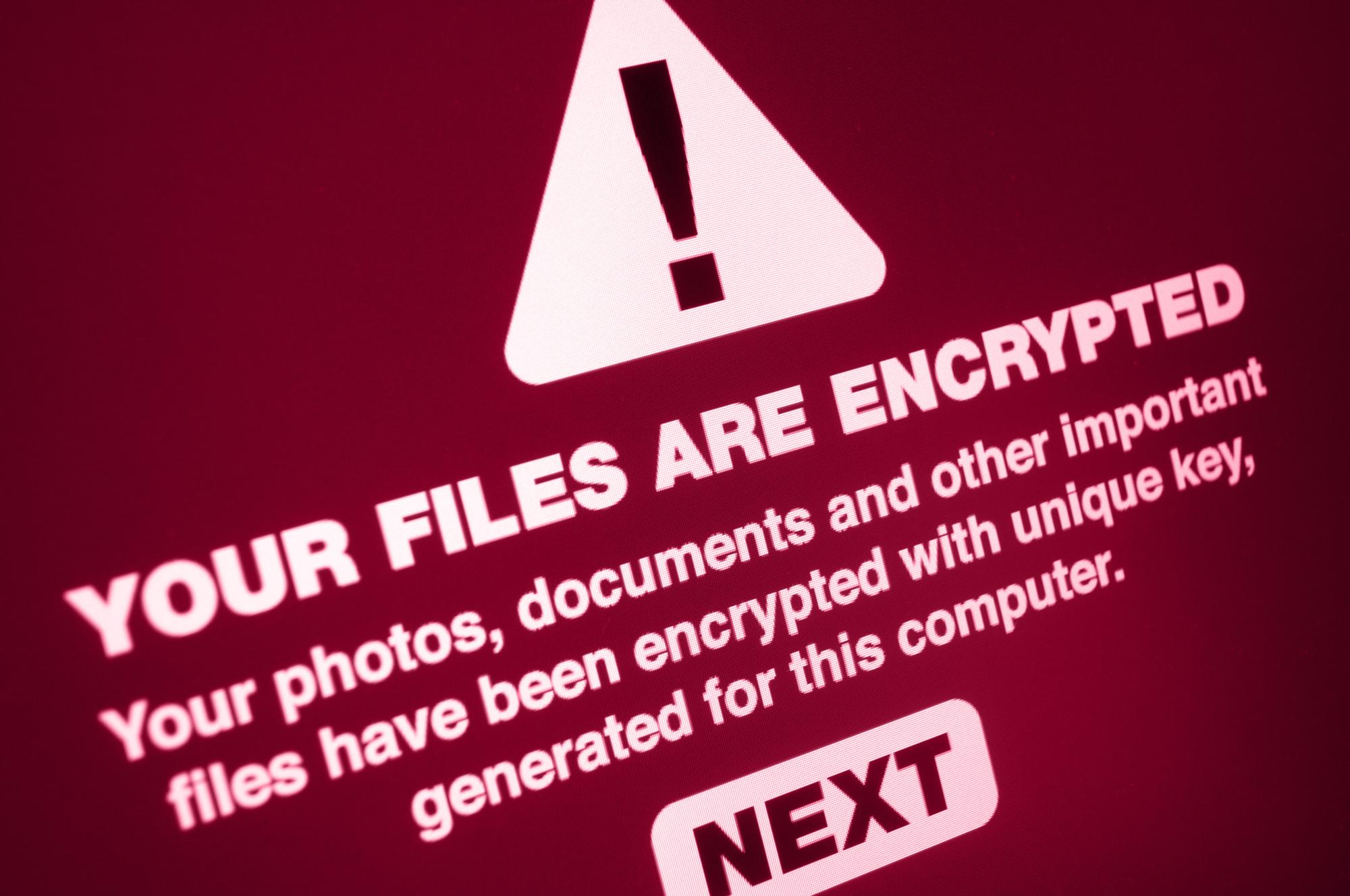
Cyber & EMP Attacks
The FBI warns that America now faces the most significant risk of cyberattacks. Yet, in some EPP Hazard Vulnerability Assessments (HVAs), cyber-attacks are not mentioned or marginalized as "unlikely risks." Hospitals that have been victims of ransomware attacks know better!
EPPs often use a scale of risks ranging from Minimum (1), Moderate (2) or Maximum (3) and view most risks as static; however, risk severity can change dramatically as crisis duration extends and new vulnerabilities emerge. Is your EPP built on the assumption that "the emergency" will last only a week or a month? Will the EPP work if the emergency lasts three months, six months, or even two years?
Long-Term Power Outages Spawn Cascade Failures
Despite emergency power circuits and healthcare backup generators, most hospitals must adequately prepare for power losses from three months to a year. They need to prepare to deal with cascade failures. Power failure can spawn water, light, heat and transportation failures, yet these vulnerabilities are rated independently, not as a risk surface, in most Hazard Vulnerability Assessment (HVA) calculations. The combination of these inter-dependencies must also be accounted for in the HVA calculation and usually isn't. Our consulting services can provide a method to do so.


Helping Americans Plan to Mitigate Threats & Increase Resilience
Improving Risk/HVA (Hazard Vulnerability Assessments)
Weather events are getting stronger and more frequent; Cat-4 and Cat-5 hurricanes are becoming common along the Eastern Seaboard. Can your facilities continue operations during sustained 175 MPH winds and 20 to 40 inches of precipitation in 2-3 days? Are any facilities vulnerable to flooding or earthquakes of magnitude 7 to 8.5? Pandemics have national and global effects. How well does your current EPP cover these? Do you have special tools like FEDECS to track items crucial to continue hospital operations? A full-scale cyberattack that disrupts the regional electrical power grid will quickly cause transportation and communication failures, leading to food, water and fuel shortages.
Risk Surfaces (4-Dimensional)
If you want to know your actual risk, forget crisis likelihood X severity = risk score assessments! They don't account for cascade failures! Please know that you are dealing with a multi-dimensional Risk Surface and begin calculating it, even if the regulatory body (State) doesn't require it.
Do what WORKS for you, not just what the State requires!
Understand your "event horizon," the point at which critical failures cease your EPP to cease functioning. Make an Action List to prevent reaching the event horizon and identify dependencies upon any third parties.
Your HVA needs to show hazards as a Risk Surface (topological Atlas) of the parameters (like shelter, access and critical resources), not just as a simple 2-dimensional table spreadsheet listing all independent vulnerabilities. If you make trivial plans, expect back outcomes & even patient lawsuits.
Dry Runs & Practice Exercises
Many EPPs are reviewed with staff only once a year, and "tabletop" crisis exercises may also be infrequent. In a real crisis, there's lots of adrenaline and unless responses are practiced and second nature, decisions will be less than optimal. MSP can identify EPP weaknesses.
The MSP team approaches Crisis/EPP from a combined administrative, nursing management, healthcare technology and mental health perspective; offering practical information to individuals, healthcare providers, skilled nursing facilities, churches and 55+ senior communities - anyone who wants to be better prepared.
MSP's Planning Perspective
